Bumped and Bruised Bottoms: Coccyx Injuries

The holidays may be over, but ‘tis still the season for slip and falls on the ice that result in tailbone and coccyx area injuries. Coccyx injuries are a common chief complaint in urgent care during this wintery, icy time of year. Classic coccydynia (aka coccyx pain) is worse when sitting and can worsen when rising from a seated position. At first glance, this seems like a straightforward chief complaint, but it lends itself to opportunities for a more nuanced discussion with patients.
What not to miss
Make sure you do a thorough evaluation of the rest of the pelvis. Just because they slipped and their coccyx region hurts the most, doesn’t mean they can’t have a concomitant fracture in the rest of their pelvis as well. Also, don’t let a slip-and-fall be a red herring – a thorough exam here usually means having the patient get undressed so you can visualize the skin. Inspection of the perineum and perianal area is essential to rule out other potential causes like pilonidal cysts, hemorrhoids, or abscesses. A donut pillow won’t fix those!
Not all coccydynia is due to trauma
Minor trauma? Easy. No trauma? This becomes more of a head-scratcher. After a thorough evaluation has convinced you the pain is isolated to the coccyx without a surrounding infectious cause, you might need to broaden your history. Does the patient perform activities that may lead to repetitive microtrauma (think motorcycles or avid Peloton-ers)? Female sex, including recent childbirth, are at higher risk of developing coccyx pain. A higher BMI leads to reduced pelvic rotation with sitting and may predispose these patients to coccydynia. Other less common atraumatic etiologies include avascular necrosis, coccyx bone spurs, sympathetic nerve pain, pelvic floor dysfunction, bursitis, or malignancies.
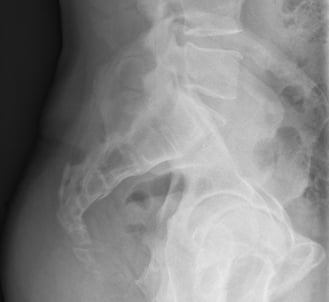
Not a simple X-ray
Sitting versus standing radiographs should be performed after 10 minutes of standing to make sure that the coccyx is in a neutral position. The sitting radiograph should be performed on a hard stool with the patient having a straight back, and thighs horizontal (you might need a footrest), and the seated radiograph performed on a hard stool. When seated, the patient should start with a flat back, thighs horizontal, and then they should lean back to the point of maximum tenderness before the X-ray is obtained.
Treatment
It’s best to advise patients that this is a slow and steady road to recovery – there is no magic healing overnight. While most of our urgent cares don’t carry donut pillows, I find it helpful to pull up a picture of what one looks like on the website of your friendly, local pharmacy or home medical equipment store so patients know what to look for. UpToDate does recommend tramadol, but just as we’ve discussed in other segments, we would recommend NSAIDs and Tylenol as initial mainstays of treatment. Physical therapy may be helpful as well. Some spicier options have shown some benefit in the literature including trials of using a capsaicin patch at the area of pain.
For more information on coccyx pain and some fun coccyx factoids, listen to Kelly Heidepriem, MD and Lance Shaull, MD on this month’s Urgent Care RAP podcast. We’d love to hear your thoughts! Leave us a comment (UC RAP > January 2024 > Chapter 8 > Discussion) and join us in discussing this important topic.
Practice-Changing Education
Experience education that goes beyond theory. Explore Hippo Education’s offerings below.


