Top 10 Tips for the Best Skin Biopsy Ever

Shave and punch biopsies are essential procedures for those who manage skin conditions and skin diseases. They can provide helpful information about undiagnosed skin lesions such as neoplasms, bullous disorders, keratoses, or dysplastic nevi. A diagnostic biopsy can also be the definitive treatment for malignant, irritated, or precancerous lesions. There's a right and a wrong way to do things, though. Here are our top 10 tips to prevent errors during skin biopsies.
Tip #1: Know your type of biopsy well, including when to use a partial biopsy vs full-thickness biopsy and incisional biopsy vs. excisional biopsy.
- Shave biopsy: commonly used for lesions that are solitary, elevated, and give the impression that a sufficient amount of tissue can be sampled using this technique.
- Punch biopsy: the best choice for most “rashes.”
- Excisional biopsy: used to remove melanocytic neoplasms or larger lesions.
- Curettage: should almost never be used for diagnostic purposes.
Tip #2: Avoid very superficial shaves. Shave biopsies are quick and lead to good cosmetic outcomes, but are prone to inadequate sampling.
Tip #3: Use a punch biopsy for rashes. It’s quick, full-thickness, and leads to good cosmetic outcomes. However, you can only sample a small area (use a 4 mm punch).
Tip #4: Use excisional biopsy for melanocytic lesions: excise the entire lesion plus 1-3 mm margins.
Tip #5: Avoid curettage for melanocytic lesions, because it distorts tissue architecture. Only use curettage if the diagnosis is certain.
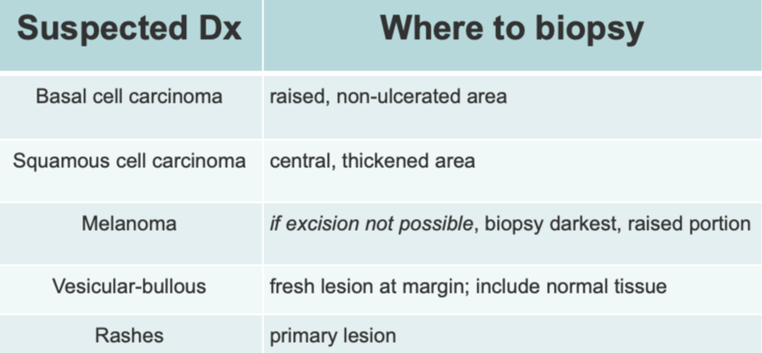
Tip #6: Know where in the lesion to biopsy.
 Tip #7: Be gentle with the specimen, and fix it right away. Aggressive handling can cause crush artifact, and prolonged time out of formalin may destroy the specimen.
Tip #7: Be gentle with the specimen, and fix it right away. Aggressive handling can cause crush artifact, and prolonged time out of formalin may destroy the specimen.
Tip #8: Photograph and document the biopsy site because some biopsies heal so well that they may be difficult to find if needed for re-excision.
Tip #9: Give the pathologist all pertinent information, including: demographics, diameter, description, duration, diseases, drugs, and differential diagnosis.
Tip #10: Know when to refer to dermatology!
- Melanocytic lesions that are difficult to biopsy
- When biopsy may compromise adjacent critical structures
- When wound closure may be an issue post-biopsy
- If uncontrolled bleeding is likely
- Lesions with non-specific histopathology that are not responding to therapy
The choice of biopsy type is made based on the working diagnosis, need for tissue, cosmesis, time, and skill of the practitioner. Follow these tips, make sure your friendly local pathologist has all the information they need to aid in diagnosis, and document the lesion location well and you will be well on your way to a spectacular skin biopsy!
For more high yield pearls and pitfalls to enhance all our skin biopsy skills, listen to Matt Zeitler, MD and Michael Baca-Atlas, MD on this month’s Primary Care RAP podcast. We’d love to hear your thoughts! Leave us a comment (PC RAP > January 2024 > Chapter 6 > Discussion) and join us in discussing this important topic.
Practice-Changing Education
Experience education that goes beyond theory. Explore Hippo Education’s offerings below.


